Hemorrhoids - a disease associated with varicose inflammation and swelling of the rectal veins in the anus. The affected areas protrude outward, they can form large knots (bumps) that interfere with the promotion and exit of stool. The disease affects both men and women, is dangerous for rupture of the veins, the addition of a secondary infection.
Classification of hemorrhoids
Depending on the location of the pathological site, 2 types of the disease are distinguished:
- External. The veins in the anus, which are covered with skin, become inflamed. For this reason, it is more difficult to damage the affected areas, they have a stronger "protection". The discomfort during defecation is less, but often an unpleasant friction is created by the linen. Complications of external hemorrhoids occur less frequently, it is easier to treat.
- Internal. The affected veins are located in the rectum above the anus, making it difficult to determine the initial stage of the disease. The vessels are covered with a thin epithelium, so they are more vulnerable to mechanical damage. The internal form of the disease often becomes chronic, it is more dangerous with complications, it is more difficult to treat.
According to the severity of the course, internal hemorrhoids are divided into 3 degrees (stages):
- Initial (1). The nodes protrude, bleed, but do not fall out.
- Moderate (2). With muscle tension (during defecation, exercise), swollen veins come out of the anus. When everything relaxes, they come back.
- Heavy (3). Knots fall, even when there is no muscle tension, they do not retract.
Symptoms
The main signs of hemorrhoids are bleeding from the anus, pain with tension in the muscles of the rectum. The complete picture depends on the stage of the disease. If nodes (separate swollen sections of the veins) appear, they look like bumps of a dark pink or purple color (rarely nearly black), are easily palpable and feel dense. The shade depends on the filling of the vessels: if blood clots have formed, the blood has collected and is unable to get out, the nodes will be dark.
internal hemorrhoids
In the first days and weeks, the disease almost does not manifest itself. It starts with edema, which is not felt unless you start probing the rectum from the inside. There are no pain receptors in that part, so a person feels no discomfort, even during the defecation process.
At an early stage of hemorrhoids, you can find out its existence only by blood drops that appear after the release of large and hard stools. Due to edema, the walls of the rectum narrow the lumen, the mucous membrane is more damaged during constipation. Important: With hemorrhoids, almost all bowel movements result in a small amount of blood appearing.
Other symptoms will follow:
- Pain during bowel movements. Severe swelling will cause a muscle spasm, so even soft stools will cause discomfort.
- Burning, itching. Due to inflammation in the rectum, a lot of mucus is formed, which irritates the tissues.
- Blood. It appears in large numbers when knots are formed. Important: with hemorrhoids, it is bright red, not dark.
- fall knots. They appear in the later stages of hemorrhoids. First, they are pulled back themselves, so they have to be "pushed" with a finger.
External
The external veins are covered with skin, which has many pain receptors. Already at an early stage of hemorrhoids, a person will experience discomfort if the vessels are swollen. Pain occurs during defecation and when cleaning the anus and with close contact of the linen with the skin. If the inflammation is severe or a blood clot forms in the vein, a large bump will form. It's easy to grope, touch causes pain.
Skin with external hemorrhoids becomes sensitive, often colliding in folds due to swelling. The process of cleaning the anus after defecation is difficult, so the risk of secondary infections increases. Blood then appears if the hemorrhoids are damaged, but there will be less of it than the formation of internal cones.
Causes
The disease is associated with impaired blood flow in the veins of the rectum, which is often caused by congestion of the pelvic organs. Due to them, the pressure in the veins increases, which swell and protrude. In most people, this occurs due to improper lifestyle and diet, but doctors do not rule out the influence of heredity, genetic vascular abnormalities and increased blood clotting.
Possible reasons why hemorrhoids appear:
- Frequent constipation - leads to tension of the veins of the anus, damage to the mucous membrane while promoting solid stool.
- Diarrhea - acute and chronic.
- Pregnancy: causes swelling, causes pressure from the growing uterus on the rectum.
- Hormonal fluctuations: cause atony of the muscles of the pelvic organs.
- Oncology of the intestine (more often - the colon).
- Postponed interventions on the rectum, less often - on the pelvic organs.
- Spinal cord injury, spinal curvature, lower back injury, sacrum, coccyx.
Additional risk factors:
- Sedentary lifestyle: causes stagnation of blood in the pelvis.
- A low-calorie, fiber-deficient diet causes constipation.
- Weight lifting causes muscle tension.
Diagnostics
Doctors review the medical history and ask clarifying questions to rule out other causes of bleeding from the anus. Hemorrhoids have symptoms similar to tumors of the digestive tract, polyps, anal fissures, prolapse of the mucous membrane.
After the doctor performs a rectal exam, feeling the lower part of the rectum with a finger. At an early stage of internal hemorrhoids, this may not give results and, at a later stage, the procedure will be postponed if the swelling is very severe and the patient's touch causes acute pain. To clarify the diagnosis and a more detailed examination of the anus, examinations are performed by a surgeon or gastroenterologist.
The following methods are applied:
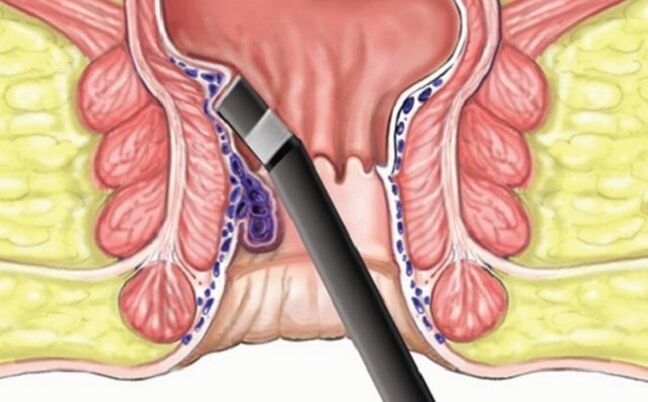
- Anoscopy. Inspection of a section of the rectum up to 10 cm long from the anus. The procedure is painless, but some patients are given local anesthesia (gel, spray).
- Sigmoidoscopy, colonoscopy. A tube is inserted into the patient's colon to rule out other causes of bleeding (tumors) and suspected lesions in the upper portions.
- magnetic resonance. Tomography is done if it is not possible to make an accurate diagnosis based on other procedures.
Laboratory research
Blood tests are rarely prescribed, it depends on the clinical picture of the disease. This is necessary if a secondary infection has appeared to determine the pathogen. They also perform an analysis in situations where bleeding from the rectum is profuse to see the level of hemoglobin, the number and activity of red blood cells. The main diagnosis does not require laboratory procedures.
Treatment
If there are no symptoms of the disease, special therapy is not required. Your doctor will advise you to change your lifestyle and diet so that the hemorrhoids do not develop, the stool becomes softer and does not damage the inflamed or swollen mucosa. The patient will be offered to move more, to do gymnastics aimed at training the muscles of the "lower press" and the small pelvis.
How to treat hemorrhoids, which cause discomfort, is determined by the doctor, given the stage of the disease. In the early stages, it is really possible to manage it only with medication. If there are many nodes, they are thrombosed and do not retract on their own, surgery may be required. In each subsequent situation the patient must follow the diet and lifestyle recommendations, because 50% of cases relapse. An exception is surgery: after it, repeated hemorrhoids occur in only 5% of patients.
Diet
The tasks of nutrition are to save a person from constipation, prevent the development of inflammation. Sources of fiber are introduced into the diet: vegetables, herbs, fresh fruit. Cereals are handled with care, especially rice: they can make the stool thick. In addition, they drink purer warm water - it does not allow feces to sinter, it also speeds up the cleansing process of the intestine. Simple carbohydrates and sugar should be discarded so as not to cause inflammation.
Medical therapy
- Laxatives. Preparations that soften the stool and relieve constipation, prevent new damage to the mucous membrane. They are drunk carefully so as not to cause loss of intestinal muscle tone and diarrhea.
- Candles with anesthetic. Relieves pain from internal hemorrhoids.
- vasoconstrictor. This is also a local therapy that reduces swelling.
- Anticoagulants. Stop bleeding.
- Hormonal preparations. They are used topically (injections) for severe inflammation.
Surgical intervention
In the last stage, hemorrhoids require surgery:
- Ligature. A tool is inserted into the anus, which throws a latex loop over the knot and tightens it. The affected area disappears after 3-4 days.
- laser surgery. The procedure with minimal trauma is almost painless, but there are many contraindications.
- Classic hemorrhoidectomy. The nodes are removed with a scalpel or a special apparatus, which then "stitches" the edges of the mucous membrane. If necessary, the doctor removes blood clots in the process.
Alternative medicine
The initial phase of external hemorrhoids involves symptomatic therapy:
- Hot baths. They are made with calendula, chamomile, sage. These herbs relieve inflammation, muscle spasm. They sit in the baths for 20 minutes up to 2-3 times a day.
- Tablets. With grated raw potatoes, aloe juice, chamomile decoction, sea buckthorn oil. They are left on gauze for 30-60 minutes.
Prevention
To avoid the question of how to cure hemorrhoids, follow simple rules:
- Move more. When sedentary, get up every 1-2 hours for 5-10 minutes. Walk in the fresh air, choose the stairs instead of the elevator, the ability to walk a few meters on foot and not drive a car.
- Watch your diet. Eat more plant foods, maintain water balance, do not abuse bread and complex carbohydrates - cereals, pasta.
























